Chronic thromboembolic pulmonary hypertension (CTEPH), similarly to other types of pulmonary hypertension (PH), reduces blood flow and increases pressure in the blood vessels of the lung1.
Breaking its name down helps us to understand what CTEPH is.
- ‘Chronic’ means a long-lasting illness.
- ‘Thromboembolic’ refers to the complete or partial blockage of a blood vessel by a blood clot that has broken away from where it was formed.
- ‘Pulmonary’ relates to the lungs.
- ‘Hypertension’ is the medical term for high blood pressure.
What causes CTEPH?
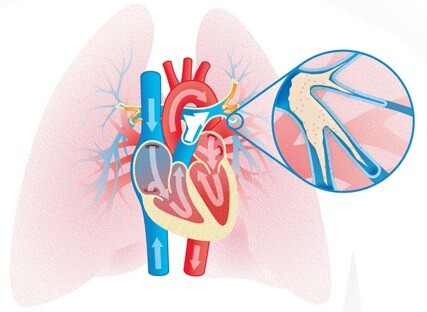
Figure 1. Chronic Thromboembolic Pulmonary Hypertension. Schematic drawing of chronic fibrotic thrombi in the pulmonary arteries, sitting at the bifurcations and spreading down to the distality.
CTEPH can be the result of blood clots that travel to the lungs (called a pulmonary embolism – PE) and block the pulmonary arteries (Figure 1). It is thought that sometimes these blood clots do not disappear completely after treatment with blood thinners (anticoagulants), and a portion may remain stuck to the wall of the arteries in the lungs. Over time, tissue forms within the clot and it becomes more fibrous, creating a blockage that stops blood flowing easily through the lungs.
These fibrous clots are characteristic of CTEPH. They are very different from blood clots and cannot be dissolved with blood thinners (Figure 2B). The presence of a number of these fibrous clots causes high blood pressure and places strain on the right side of the heart, causing it to enlarge and weaken. If left untreated, this may eventually lead to right heart failure.
There is no single gene causing CTEPH.
CTEPH is the only type of PH that can potentially be cured.
How many are affected by CTEPH?
CTEPH is estimated to affect about 43 to 50 cases per million people in Europe 2. CTEPH is defined as ‘Group 4’ in the World Health Organization (WHO) clinical classification of PH 3 (see classification for further information).
How is CTEPH diagnosed?
CTEPH is most commonly diagnosed when a patient presents with acute pulmonary embolism (PE) that is unusually severe but relatively well tolerated by the patient, with a big right heart, and a wide central pulmonary artery by computed tomography pulmonary angiography. However, about one third of patients has never had any acute PE before they present with CTEPH. Echocardiography usually demonstrates an enlarged right chamber, but sometimes this enlargement is very mild or even absent. A screening test called a ventilation-perfusion lung scan should be carried out on all patients with pulmonary hypertension to assess whether or not they may have CTEPH. Proof is achieved by an invasive right heart catheterization including pulmonary angiography, or direct injection angiography.
Surgery for CTEPH
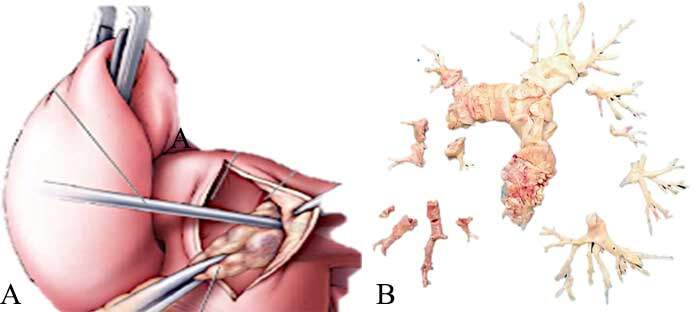
Figure 2. Pulmonary Endarterectomy for Chronic Thromboembolic Pulmonary Hypertension. Schematic drawing in panel A illustrating the dissection of the pulmonary artery in the layer of adjacent fibrotic thrombus. Panel B shows a surgical specimen with very little fresh red clot. The majority of the obstructions is white and fibrotic.
An operation called a pulmonary endarterectomy (PEA) can be performed to remove the fibrous blockage(s) from the lung (Figure 2). PEA surgery is only carried out by a small number of highly skilled surgeons in the world. Quality of life and life expectancy improve for many people with CTEPH after PEA 4, and mean pulmonary artery pressure goes down to <30mmHg in many cases.
Before deciding if patients with CTEPH are suitable for PEA, they need to be thoroughly assessed by a CTEPH team at a specialist CTEPH center 3. After PEA surgery, patients still need to have regular medical tests and will need blood-thinning medication for the rest of their lives. It is not clear today whether the new anticoagulants are as effective as vitamin K antagonists, for example warfarin. Even after surgery, CTEPH may persist or return at a later date, and so further treatment may be required.
Balloon Pulmonary Angioplasty for CTEPH
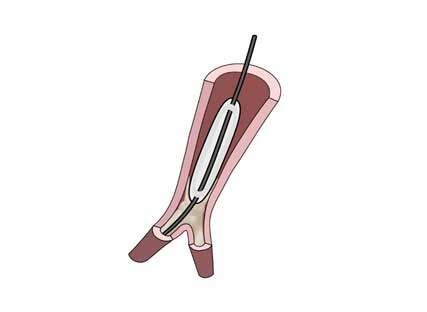
Figure 3. Balloon Pulmonary Angioplasty for Chronic Thromboembolic Pulmonary Hypertension. Schematic drawing illustrating an inflated balloon on a guide wire breaking a bifurcational web. Antegrade flow to the distality will be restored.
Worldwide at least 50% of CTEPH patients do not undergo PEA. One reason is that the obstructions are too distal, another reason is that PEA is too risky, for example in an elderly and frail patient. For these previous interventional no-option patients balloon pulmonary angioplasty (BPA) has been refined by Japanese interventionists 5. BPA uses conventional angioplasty guiding catheters, balloons and wires 6 (Figure 3). European and American registries illustrate that BPA is able to lower mean pulmonary artery pressure by one third, and pulmonary vascular resistance by half. BPA is possible in patients with persistent or recurrent CTEPH following PEA. BPA may be safer when combined with medical treatments.
Medical treatment for CTEPH
Surgery should always be considered first for someone with CTEPH, and the indication should be discussed in a CTEPH team 3 before medical therapy is started or BPA is performed. However, if surgery is not an option and in patients with persistent or recurrent CTEPH following PEA, the soluble guanylate cyclase stimulator riociguat, and since recently, subcutaneous treprostinil in Europe have been approved by health authorities for patients with inoperable CTEPH and those with persistent or recurrent CTEPH following PEA.
The future for CTEPH
In recent years, advances in imaging technology have led to improvements in the diagnosis of CTEPH. BPA has further enhanced the understanding of CTEPH. First, invasive intravascular imaging has disclosed many more cases than were initially diagnosed. Second, a new understanding of the completeness of an interventional procedure have been gained. For example, Japanese patients have seen near normalization of pulmonary pressures through repeated procedures. Moreover, medical treatment will be improved in the future, presumable as combination treatments including riociguat, to improve exercise capacity.
As we stand today, PEA, PBA and medical treatment are being employed in complementarity by CTEPH experts, for the most benefit of their patients.
Further information and educational materials on CTEPH can be found in the section PH: It’s personal.
Dr. Irene M Lang, Professor of Vascular Biology
Department of Cardiology
AKH-Vienna, Medical University of Vienna
AUSTRIA
Last medical update: 05/30/2020
Sources
- Lang IM and Madani M. Update on chronic thromboembolic pulmonary hypertension. Circulation. 2014;130:508-18.
- Cottin V, Avot D, Levy-Bachelot L, Baxter CA, Ramey DR, Catella L, Benard S, Sitbon O and Teal S. Identifying chronic thromboembolic pulmonary hypertension through the French national hospital discharge database. PloS one. 2019;14:e0214649.
- Kim NH, Delcroix M, Jais X, Madani MM, Matsubara H, Mayer E, Ogo T, Tapson VF, Ghofrani HA and Jenkins DP. Chronic thromboembolic pulmonary hypertension. The European respiratory journal. 2019;53.
- Mahmud E, Madani MM, Kim NH, Poch D, Ang L, Behnamfar O, Patel MP and Auger WR. Chronic Thromboembolic Pulmonary Hypertension: Evolving Therapeutic Approaches for Operable and Inoperable Disease. Journal of the American College of Cardiology. 2018;71:2468-2486.
- Mizoguchi H, Ogawa A, Munemasa M, Mikouchi H, Ito H and Matsubara H. Refined balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic pulmonary hypertension. Circulation Cardiovascular interventions. 2012;5:748-55.
- Lang I, Meyer BC, Ogo T, Matsubara H, Kurzyna M, Ghofrani HA, Mayer E and Brenot P. Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. European respiratory review : an official journal of the European Respiratory Society. 2017;26.
- UK National Health Service. Service Specification and Standards – Pulmonary Thromboendarterectomy. Available from: http://www.webarchive.org.uk/wayback/archive/20130325152542/http:/www.specialisedservices.nhs.uk/document/service-specification-standards-pulmonary-endarterectomy/search:true (accessed August 2014).